The global conversation around obesity is shifting as a recent report calls for a new definition that considers overall health rather than solely relying on the Body Mass Index (BMI) metric. Published in The Lancet Diabetes & Endocrinology journal and supported by over 50 medical professionals globally, the report argues that many individuals currently classed as obese may not be unhealthy or require strict medical interventions.
Instead, experts suggest that those suffering chronic illnesses linked to their weight should be classified as "clinical obesity,” while those without any health complications be recognized as having "pre-clinical obesity." This nuanced approach aims to provide a more personalized understanding of obesity, allowing for more appropriate care and treatment options.
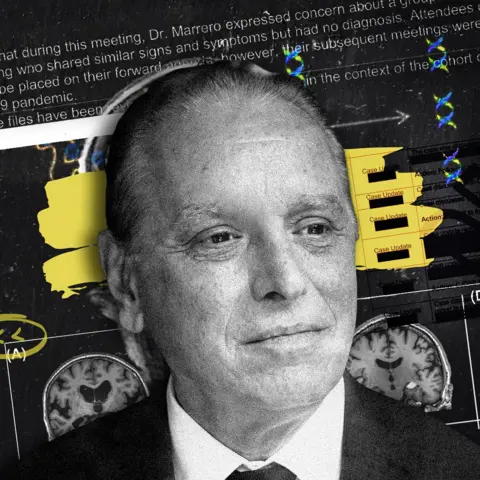
According to Professor Francesco Rubino from King’s College London, who led the expert group, "Obesity is a spectrum,” emphasizing that many individuals with excess fat can maintain a healthy, functional life. Conversely, some face severe health issues that impact their mobility and quality of life.
Current practices across numerous countries define obesity through a BMI over 30, a figure derived from height and weight measurements. However, the report critiques this method, stating that it does not truly reflect a person's health status or the types of fat they carry. The authors advocate for assessments that consider relevant health indicators such as heart disease, diabetes, or mobility issues to classify obesity accurately and assign proper treatment plans.
The report stresses the need for a fresh model focusing on the influence of obesity on organ health rather than merely relying on BMI. This model identifies those who may not need aggressive medical interventions but can benefit from lifestyle changes and regular monitoring, thereby reducing health risks over time.
Prof. Louise Baur of the University of Sydney emphasized that this redefined approach would not only enhance care for adults but also allow for better management of childhood obesity cases, decreasing the likelihood of overdiagnosis and unnecessary treatment.
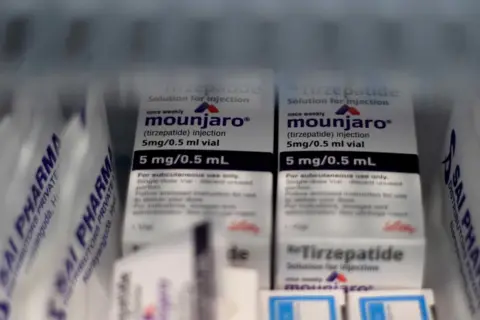
As prescription weight-loss medications gain popularity, the necessity for such a reframing of obesity definitions becomes increasingly important. Despite the push for better classification, experts fear that financial limitations within health systems will primarily benefit clinically obese patients, while those classified as pre-clinical might not receive adequate focus or resources. Prof. Jim Mann from New Zealand highlighted this concern, stressing that funding constraints may prioritize care for more severely impacted individuals.
This progressive report lays the groundwork for treating obesity with the urgency and understanding similar to other chronic illnesses, marking a pivotal moment in the fight against obesity globally.
Instead, experts suggest that those suffering chronic illnesses linked to their weight should be classified as "clinical obesity,” while those without any health complications be recognized as having "pre-clinical obesity." This nuanced approach aims to provide a more personalized understanding of obesity, allowing for more appropriate care and treatment options.
According to Professor Francesco Rubino from King’s College London, who led the expert group, "Obesity is a spectrum,” emphasizing that many individuals with excess fat can maintain a healthy, functional life. Conversely, some face severe health issues that impact their mobility and quality of life.
Current practices across numerous countries define obesity through a BMI over 30, a figure derived from height and weight measurements. However, the report critiques this method, stating that it does not truly reflect a person's health status or the types of fat they carry. The authors advocate for assessments that consider relevant health indicators such as heart disease, diabetes, or mobility issues to classify obesity accurately and assign proper treatment plans.
The report stresses the need for a fresh model focusing on the influence of obesity on organ health rather than merely relying on BMI. This model identifies those who may not need aggressive medical interventions but can benefit from lifestyle changes and regular monitoring, thereby reducing health risks over time.
Prof. Louise Baur of the University of Sydney emphasized that this redefined approach would not only enhance care for adults but also allow for better management of childhood obesity cases, decreasing the likelihood of overdiagnosis and unnecessary treatment.
As prescription weight-loss medications gain popularity, the necessity for such a reframing of obesity definitions becomes increasingly important. Despite the push for better classification, experts fear that financial limitations within health systems will primarily benefit clinically obese patients, while those classified as pre-clinical might not receive adequate focus or resources. Prof. Jim Mann from New Zealand highlighted this concern, stressing that funding constraints may prioritize care for more severely impacted individuals.
This progressive report lays the groundwork for treating obesity with the urgency and understanding similar to other chronic illnesses, marking a pivotal moment in the fight against obesity globally.